Media ID: 55384665
Caption:

Media ID: 55384532
Caption:

Media ID: 55382591
Caption:

Media ID: 55382271
Caption:

Media ID: 55380911
Caption:
Caption:
FILE PHOTO: The Nutrition Facts label is seen on a box of Pop Tarts at a store in New York February 27, 2014. REUTERS/Brendan McDermid

Caption:
A nurse vaccinates a patient as part of the start of the seasonal influenza vaccination campaign in Nice, southeastern France, October 21, 2015. REUTERS/Eric Gaillard

Oxford University to Test Universal Flu Vaccine in World First
A seasonal flu vaccine that would be the first in the world to fight all types of the virus is to be tested in a two-year clinical trial involving more than 2,000 patients by researchers in Oxford. The so-called universal vaccine was developed by Oxford University’s...Caption:
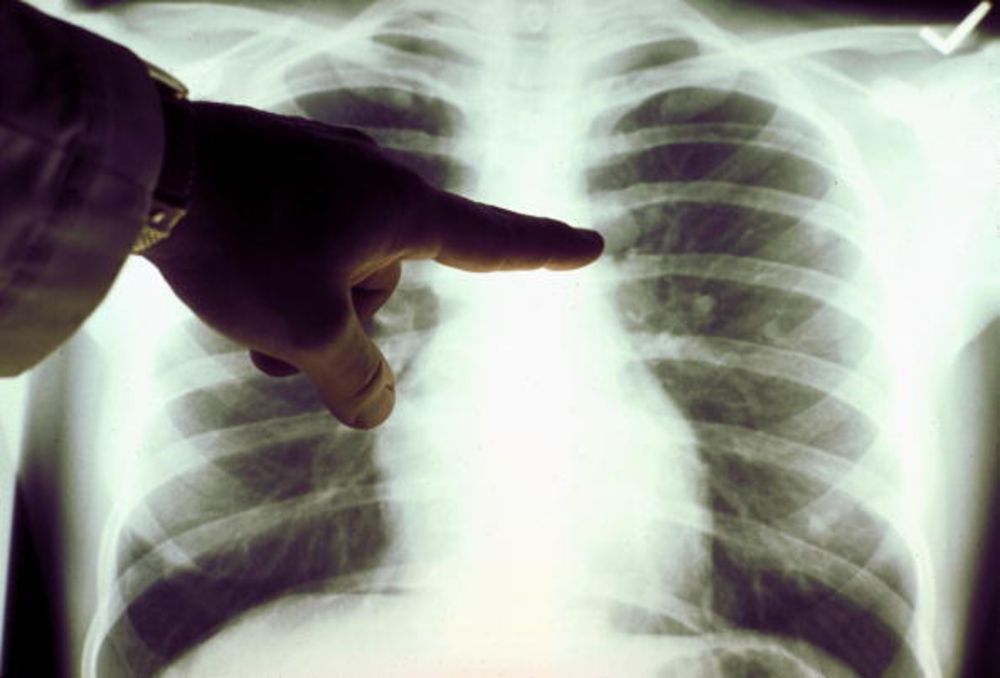
The camera has been designed to help doctors track medical tools known as endoscopes within the body

New Camera Sees Through Human Body By Detecting Light
London- Scientists have developed a camera that can see through the human body. The device has been designed to help doctors track medical tools, known as endoscopes, during internal examinations. Until now, medics have had to rely on expensive scans, such as X-rays,...Caption:
A man drinks a soft drink at a store in Mexico City September 9, 2013. REUTERS/Edgard Garrido/Files

Counting on Fewer Calories
Can curbing your usual daily calorie intake by 10% improve health and longevity? There is a saying: “The less you eat, the longer you live.” The rising rates of obesity have shown that Americans consume more than necessary, and cutting back on calories may...Caption:
A tumor is a trove of data. Photograph: American Cancer Society/Getty Images